Kidney failure is a major global health concern. The two main treatment are hemodialysis and peritoneal dialysis, each with a special strategy and set of factors to take into account.
Hemodialysis
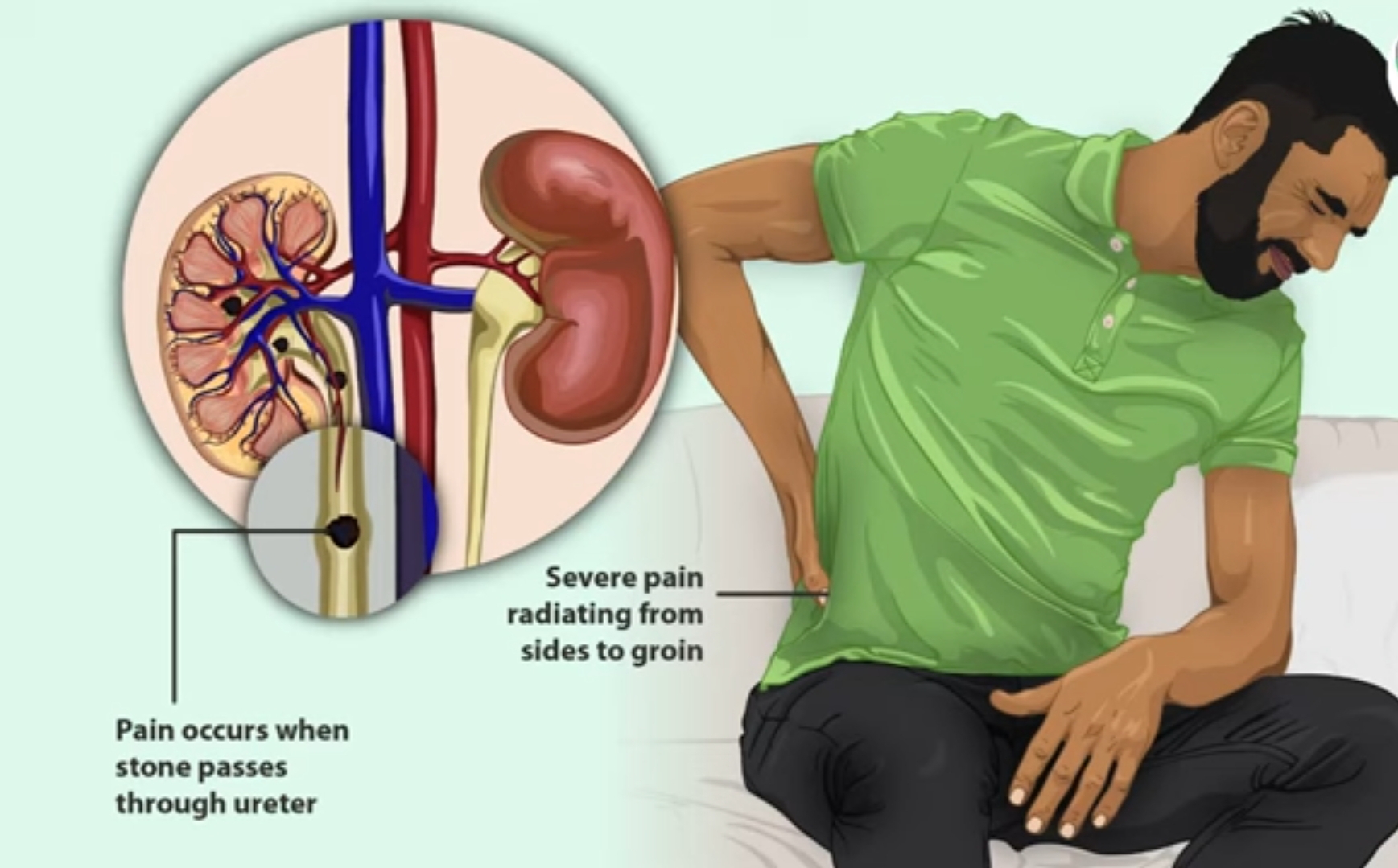
Hemodialysis: Hemodialysis is the procedure of utilizing a dialysis machine to remove waste materials and extra fluid from the blood. Hemodialysis involves pumping the patient’s blood outside the body via a dialyser, an artificial kidney that serves as a filter. When the dialyzer returns the body’s cleaned blood, it eliminates pollutants and keeps the electrolyte balance in check.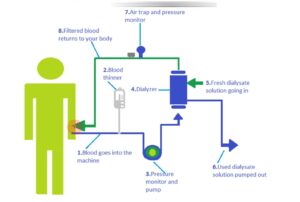
Hemodialysis treatments are usually administered in hospitals or specialty clinics and call for frequent, multi-hour sessions, frequently multiple times a week. During the procedure, patients may feel some discomfort, including as blood pressure changes and sporadic cramping in their muscles.
Peritoneal
peritoneal dialysis makes use of the peritoneum a membrane that lines the abdominal cavity—as a built-in filter. A catheter is used to insert dialysate, a cleansing solution, into the abdominal cavity during peritoneal dialysis. Diffusion and osmosis allow waste materials and extra fluid to exit the bloodstream and enter the dialysate solution.
Following a dwell time, the accumulated toxins are removed together with the spent dialysate and replaced with new solution.Compared to hemodialysis, peritoneal dialysis is more flexible because it may be done at home, giving patients more freedom and less limitations on their regular activities. However, because of the catheter, there is a danger of infection and it necessitates close attention to treatment guidelines.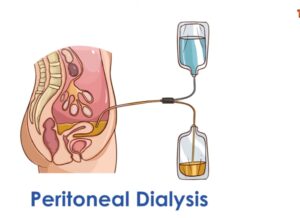
Procedure for Hemodialysis:
Vascular Access:
Prior to beginning hemodialysis, a vascular access point must be established. This is typically done by implanting a synthetic tube known as a graft or by surgically uniting an artery and a vein to form a fistula. A catheter may be used as a temporary access method in certain situations.The dialyzer, an artificial kidney, is attached to the patient via a hemodialysis machine, which uses tubing to flow blood from the body to the device. Semi-permeable membranes in the dialyzer remove surplus and waste fluid from the circulation.
Blood Filtration:
Toxins, waste materials, and extra fluid diffuse across the membrane of the dialyzer as the blood flows past it, creating a dialysate solution that aids in preserving the right electrolyte balance.
Return of Purified Blood: A second pair of tubing is used to deliver the purified blood back to the patient’s body.
Monitoring
The patient’s vital indicators, such as blood pressure and heart rate, are continuously observed during the hemodialysis session. Depending on the patient’s condition, the dialysis machine settings may need to be changed.
Session End: The patient is disconnected from the machine and the vascular access site is appropriately cared for once the hemodialysis session has lasted the full amount of time that was prescribed.
Procedure for Peritoneal Dialysis:
Catheter Insertion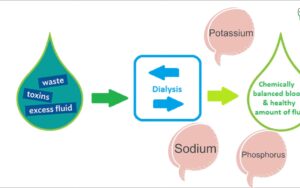
The patient has a soft, flexible catheter surgically placed inside of their abdomen. During peritoneal dialysis, this catheter is used as a conduit to add and remove dialysate fluid.
Dialysate Preparation:
In accordance with the patient’s treatment plan, a specific volume of dialysate solution is made. Glucose and electrolytes in the solution aid in removing waste materials and extra fluid from the circulation.
Dwell Phase:
Using a catheter, the dialysate solution is administered into the abdominal cavity. After entering the cavity, it stays there for a predetermined amount of time, usually several hours, allowing toxins and waste materials to diffuse and osmotically enter the dialysate solution from the blood vessels.
Drainage Phase:
The utilized dialysate, which now contains waste materials and extra fluid, is drained from the abdomen through the catheter and into a collection bag following the dwell period.
Cycling: In order to accomplish peritoneal dialysis, a cycle of infusion, dwell, and drainage is usually followed several times during the day. The patient’s prescription and treatment plan determine how often and how long peritoneal dialysis exchanges will occur.
Catheter Care: To avoid infection and guarantee the efficacy of peritoneal dialysis treatments, the catheter site needs to be well maintained.
Dietary Guidelines for Patients Receiving Dialysis:
Controlled Fluid Intake:
To avoid fluid overload and related problems including elevated blood pressure and fluid accumulation, stick to the fluid consumption guidelines provided by your doctor.Keep an eye on your fluid consumption by measuring out liquids and steering clear of items that are high in water.
Monitoring Potassium Intake
Eat less of foods high in potassium, such as oranges, potatoes, bananas, tomatoes, and dried fruits.Pick low-potassium substitutes such as cabbage, green beans, berries, apples, and grapes.
Track your intake of phosphorus:
Limit items high in phosphorus, such as processed foods, dairy products, nuts, and seeds, as well as whole grains.To regulate the amount of phosphorus in your blood, choose to take binders as directed by your doctor.
Reduce Your Sodium Intake:
Cut back on sodium to help control blood pressure and fluid retention.Steer clear of packaged and processed foods, canned soups, fatty snacks, and sodium-rich condiments.Instead of adding salt to increase flavor, use herbs, spices, and lemon juice.
Control Your Protein Consumption:
Eat a reasonable amount of high-quality protein to help maintain the health of your muscles and reduce waste accumulation.Pick lean protein sources including tofu, fish, poultry, and eggs.Eat less red meat and dairy products and other meals high in protein since too much protein can damage the kidneys.
Track the balance of fluids and electrolytes:
Take caution when consuming meals like soups, gelatin desserts, and ice cream that may contain concealed fluids.Keep an eye out for foods and drinks that are high in electrolytes, such as sports drinks, specific fruits, and vegetables.
Dialysate Preparation:
To create a customized meal plan that takes into account your medical needs, dialysis schedule, and nutritional requirements, speak with a certified dietitian who specializes in renal disease.To determine your nutritional status and make the required adjustments, stick to your eating plan and schedule frequent follow-up meetings.
When is hemodialysis required?
If your kidneys are unable to filter enough fluid and waste from your blood to maintain your health, you will require dialysis. This often occurs when your kidney function is between 10 and 15 percent reduced. You can have symptoms like exhaustion, edema, nausea, and vomiting. Even so, you may still have a high blood waste level that could be harmful to your health even if you don’t now exhibit any of these symptoms. The best person to advise you on when to start dialing is your doctor.
How is my blood cleaned by the dialyser?
There are two sections to the dialyzer, or filter: one holds your blood, and the other has dialysate, a cleaning solution. These two sections are separated by a thin membrane. Because blood cells and other essential components are too large to travel through the membrane, they stay in your blood. Smaller waste materials in the blood are washed away by passing through the membrane, including potassium, creatinine, urea, and excess fluid.
How much time does each hemodialysis session last?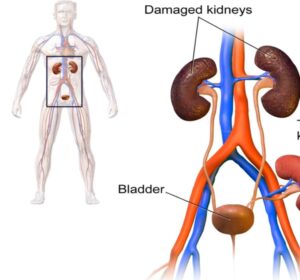
Hemodialysis is typically performed in a dialysis facility three times a week mostly depends on the condition of kidney functional of the patient ,it usually takes four hours at a time. Hemodialysis patients who opt for at-home therapy may undergo dialysis 4–7 times a week for a lesser duration each time.
You will receive a prescription from your doctor indicating the extent of your treatment requirements. According to studies, receiving the recommended dosage of dialysis prolongs your life, enhances your general health, and keeps you out of the hospital. In order to make sure you are receiving the appropriate dosage of dialysis, your dialysis care team will use monthly lab tests to monitor your therapy. Urea is one of the tools your dialysis care team may employ.
I have renal problems, can dialysis help?
Dialysis may only be required briefly until the kidneys recover in certain cases of abrupt or acute renal failure. Your kidneys do not get better from chronic kidney disease, though, and unless you are able to get a kidney transplant, you will require dialysis for the remainder of your life if kidney failure develops over time.
Will receiving hemodialysis hurt me?
The needles used to insert your fistula or graft may hurt when you first start hemodialysis. Most patients eventually adjust to this. Throughout your treatment, your dialysis care team will make every effort to keep you as comfortable as possible. Although cramps, headaches, nausea, or dizziness are uncommon symptoms, if you have any of them, see if any of the following actions can help:* Reduce the rate at which you remove fluid, as this may lengthen your dialysis session.*Up the salt content of your dialysate.* Examine the drugs you use for high blood pressure.* Modify your target weight, or dry weight.* Let the dialysate cool slightly.*Take a prescription drug to help prevent hypotension during dialysis
How is dialysis performed peritoneally?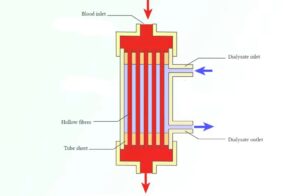
Surgery is used to insert a catheter—a soft plastic tube—into your abdomen. Using this catheter, a sterile cleansing solution is injected into your stomach. Through the catheter, the fluid exits your body once the filtering procedure is complete.
What benefits and drawbacks come with receiving peritoneal dialysis?
Compared to hemodialysis, several medical professionals believe that CAPD and APD offer a number of advantages. You can more readily control excess fluid with continuous dialysis, which may lessen the strain on your heart and blood vessels. You can consume more food and take fewer prescription drugs. It’s simpler to work or travel, and you can do more of your regular tasks.
Nevertheless, peritoneal dialysis might not be suitable for certain individuals. Some people’s bellies may make peritoneal dialysis difficult or impossible, especially those who are severely obese or have had numerous previous abdominal procedures. Abdominal infection, or peritonitis, is a rare complication, even though it ought to be rare and involve the right safety measures. You should note that peritoneal dialysis is typically a daily process, similar to how the kidney functions, and may be more mild when it comes to removing fluid from the body when choosing the form of therapy.
It has been demonstrated that hemodialysis is not superior than peritoneal dialysis as an effective kind of dialysis.Not everyone is a candidate for peritoneal dialysis. Individuals need to be properly trained and capable of carrying out each therapeutic process. Another option is to engage a qualified assistant.
conclusion
Whereas hemodialysis, which is carried out in specialty clinics or hospitals, circulates blood through a dialysis machine, peritoneal dialysis gives patients the ease of receiving treatment at home by using their peritoneum as a natural filter. From vascular access management in hemodialysis to catheter care and infection control in peritoneal dialysis, each modality has its own special issues and difficulties.